Semaglutide (Trusted Source) is one of the GLP-1 receptor agonist class of drugs that is being used more and more. At the moment, the FDA has approved the name brands Rybelsus and Ozempic for the treatment of diabetes and Wegovy is used to help people lose weight.
- A GLP-1 agonist drug called semaglutide can help control diabetes and reduce body weight.
- A further potential health benefit of semaglutide is also of interest, experts say.
- Semaglutide may help improve liver health in patients with steatohepatitis, a severe form of fatty liver disease associated with metabolic dysfunction, a study suggests.
Other uses of semaglutide are also of interest, say experts. Research on the medication was recently moved forward by a study looking at the side effects of the drug in patients with metabolic dysfunction-associated steatohepatitis, a liver disease, and the material was published in The New England Journal of Medicine.
Semaglutide enhances liver function.
This study included individuals with metabolic dysfunction–associated steatohepatitis (MASH) and is a phase 3 clinical trial that describes MASH (severe form of what was formerly termed nonalcoholic fatty liver disease).
MASH may also involve inflammation, steatosis, or the accumulation of fat in the liver, and damage to the liver’s cells, the study said. Steatohepatitis, which leads to inflammation and fat accumulation in the liver, can then lead to fibrosis, or tissue scarring.
The participants in this study were from 37 countries and in hundreds of clinical settings. The first round of the trial is closed, according to the latest results reported.
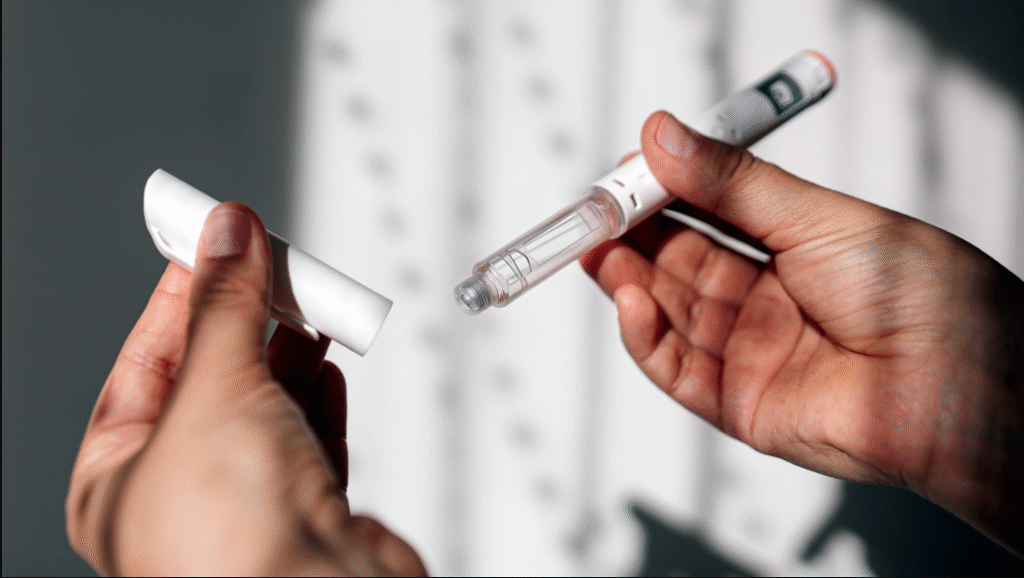
Of the patients, 266 were given a placebo and 534 received semaglutide. The study was conducted over 72 weeks, and participants underwent a 16-week dose increase course, and received weekly injections of semaglutide at a dose of 2.4 mg.
Every patient had fibrosis and steatohepatitis and was at least 18 years of age. Patients with chronic liver disease other than nonalcoholic fatty liver disease were not included in the study. Other prespecified factors were e. g., excessive alcohol intake and the use of GLP-1 receptor agonists for 3 months before screening, as well as regular MASH care. Two liver biopsies were carried out on all patients to evaluate the clinical effect of semaglutide.
Around 73% of the patients were obese, and 56% had type 2 diabetes.
Two primary outcomes were examined by the researchers: resolution of steatohepatitis in which the liver fibrosis did not worsen and improvement of fibrosis in which the liver fibrosis did not worsen The research team also assessed participants’ weight fluctuations, discomfort, adverse events and lab data.
The participants presumably had more benefit from semaglutide than from the placebo. Semaglutide effectively resolved steatohepatitis in over 63% of patients, demonstrating no worsening of their fibrosis; however, this result only existed in 34. 3% of participants in the placebo group.
Additionally, compared with 22. 4% for placebo, a mean reduction in liver fibrosis (36 8%) did not lead to a worsening of steatohepatitis at the same time. Subtracting other constructs such as age, diabetes and severity of fibrosis showed similar results.
Some patients also experienced a lower fibrosis score and remission of steatohepatitis (about 33% of the semaglutide group and 16% of the placebo group).
The effects of semaglutide on pain, inflammation, and weight loss
Also, the semaglutide group showed an average body weight loss of 10. 5%, compared with the placebo group (average body weight loss of 2%), and the semaglutide group also appeared to have less discomfort than the placebo group (this difference did not reach statistical significance).
Also, members of the semaglutide group showed better results in non-invasive tests: a larger number of semaglutide users – compared with placebo – had reduced liver stiffness and higher liver fibrosis scores.
Further, the semaglutide group showed improved insulin sensitivity and larger reductions in cholesterol and systemic inflammation.
About 80% of placebo recipients experienced an adverse event while 86% of those on semaglutide did, the researchers said. Also, compared with placebo, semaglutide had higher gastrointestinal side effects such as nausea and constipation, they said. “No new or liver-related safety encodings surfaced, ” the researchers said.
Limitations of the study
The study found that, overall, semaglutide may help patients with MASH with better liver outcomes, though there are some limitations.
First, the study involved very few Black people and not many very thin people. We still don’t know what semaglutide can do for thin people with MASH and other studies will likely need more people in them. We did not have access to biomarkers of alcohol intake, and the researchers acknowledged that “the likelihood of someone responding to treatment will depend on what is genetic.”
Overall, the findings of this study suggest that semaglutide may help some patients with MASH achieve improved liver outcomes. Just like drugs there are trade-offs.
First of all, there were not a lot of Black people in the study and not many thin people either. What might be the benefit of semaglutide use in cases of slim people with MASH is not clear, so it may be necessary for future studies to be more variable. Biomarkers for alcohol consumption are not available to the researchers, however. They also recognise that someone’s treatment response may be affected by genetics.
There will be much more follow-up on this one experiment (as it is still active), and we will start by emphasizing survival without cirrhosis. For the sake of keeping the trial honest, the researchers didn’t disclose certain clinical outcome data in this report: The part of the study that included 800 randomized participants had nothing to do with how well people did after taking semaglutide, a placebo, or specific medication changes. It also missed some data points.
Semaglutide provided comprehensive success in tackling “liver disease and associated cardiometabolic illness” — and addressed key metabolic dysfunction factors that create liver damage, researchers said.
The results of this study might be the consequence of weight loss. In an interview with Medical News Today, Mir Ali, MD, a board-certified general surgeon, bariatric surgeon, and medical director of the MemorialCare Surgical Weight Loss Center at Orange Coast Medical Center in Fountain Valley, CA, expressed the following:
This study shown that using semaglutide reduced MASH; however, since obesity is the main cause of MASH, I think this is more a result of weight loss than a direct result of the drug. Our surgical weight loss patients experience a considerable improvement in MASH, and this improvement appears to be directly correlated with weight loss. The therapeutic ramifications are that this indicates an additional advantage of semaglutide usage for weight loss.
Is it possible to treat liver diseases with semaglutide?
Another possible benefit of semaglutide is that it may be able to help people with MASH, this study suggests.
MNU was informed by Ian Storch, DO (osteopathic physician who practices internal medicine and gastroenterology, a member of the American Osteopathic Association). Ian Storch did not take part in the study.
“Metabolic Associated Hepatitis (MASH) has been largely neglected in the past for the following reasons: first, it is difficult and expensive to develop affordable non-invasive imaging techniques for measuring fibrosis and second, there are no clinically effective therapies. Another major step forward in our quest to prevent this slow-moving but fatal disease is the NEJM study reports that semaglutide may be effective in the treatment of patients with advanced inflammation and fibrosis in MASH.




2 thoughts on “Semaglutide (A diabetes medication and weight loss drug) can be used to treat liver disease in 2025”