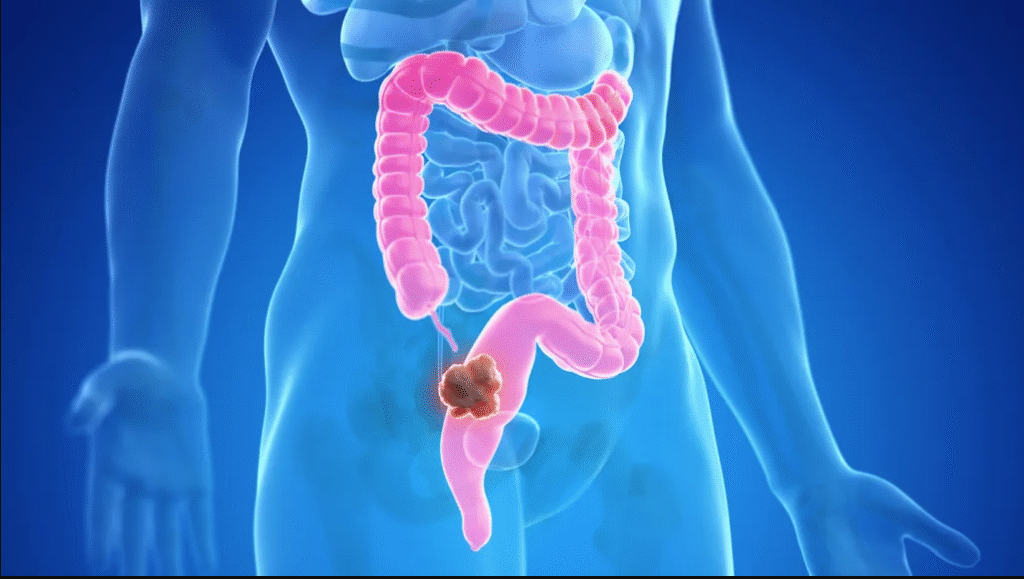
As the third most common cancer and the second leading cause of death from cancer, colorectal cancer (CRC) is a major global health issue. CRC has historically been regarded as an age-related disease that mostly affects people over 50. This trend was largely influenced by lifestyle factors and the implementation of widespread screening programs, which contributed to declining incidence rates among older adults in many high-income countries.
However, a worrying trend has emerged in recent decades, with an increase in CRC incidence among younger adults (those under 50). This rise is especially noticeable in countries with high incomes, such as Australia, parts of Europe, and the United States (U.S.), but it is also emerging in Asian and Latin American nations.
This article explores the rising incidence of CRC among young adults, investigating possible causes, risk factors, and preventative strategies.
The upward trend
CRC is a growing concern among younger populations in the United States. While overall CRC mortality has decreased, the number of cases among individuals under 50 has steadily increased, according to the American Cancer Society.
About 19,550 people under the age of 50 were diagnosed with CRC in 2023, and this age group was responsible for 3,750 deaths. The proportion of CRC cases in individuals under 55 has nearly doubled from 11% in 1995 to 20% in 2019.2
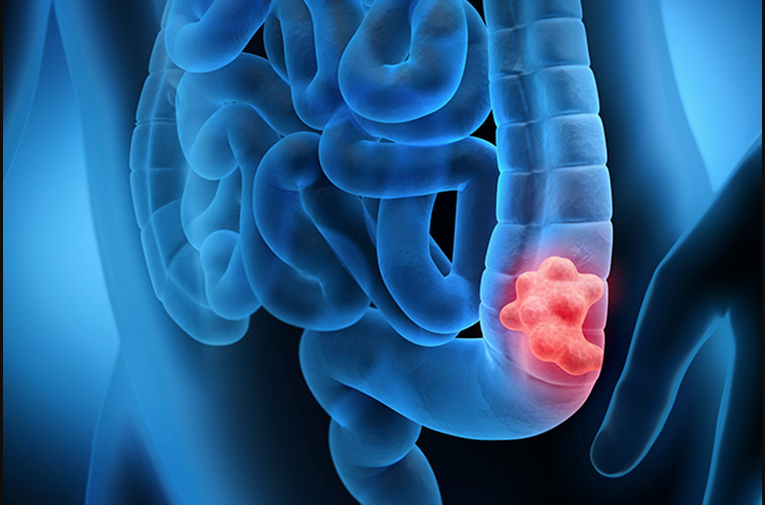
More diagnoses at advanced stages accompany this shift. From 2010 onward, regional-stage cases increased by 2%-3% annually in those under 65 and distant-stage cases by 0.5%-3%. The trend reverses previous progress in early-stage detection due to widespread screening. Rectal cancer cases, in particular, have risen, with their share of total Colorectal Cancer diagnoses growing from 27% in 1995 to 31% in 2019.2
Despite overall mortality declining, younger individuals are experiencing an increase in Colorectal Cancer deaths by 0.5%-3% annually. Changes in lifestyle, diet, obesity, and genetics may all be to blame for this rise, but the reasons are still unknown. Addressing this growing crisis requires improved early detection strategies and equitable access to screening and treatment, particularly for high-risk groups.2
Possible reasons
Epidemiological data show that Westernized diets high in red and processed meats and low in fiber- contribute significantly to Colorectal Cancer risk. Consuming a lot of red meat makes the gut microbiota produce more metabolites like trimethylamine-N-oxide (TMAO) and secondary bile acids. These metabolites cause inflammation and cancer to grow. In contrast, fiber-rich diets enhance short-chain fatty acid (SCFA) production, reducing inflammation and strengthening the gut barrier, thus lowering CRC risk.3,4
CRC development relies heavily on the gut microbiome. Dysbiosis (an imbalance in gut microbial composition) has been linked to Colorectal Cancer. Specific microbial strains, such as Bacteroides fragilis and Fusobacterium nucleatum, have been found to promote tumorigenesis by triggering inflammatory pathways and evading the immune system. On the other hand, beneficial bacteria like Bifidobacterium and Faecalibacterium prausnitzii assist in maintaining homeostasis in the gut and may protect against CRC.3,4 Lifestyle risk factors for Colorectal Cancer include obesity, inactivity, smoking, and excessive alcohol consumption. Obesity alters gut microbiota composition and increases systemic inflammation, which fosters a pro-carcinogenic environment.
On the other hand, physical activity has been shown to lower the risk of CRC and positively alter the microbiome. Additionally, exposures to the environment, such as overuse of antibiotics, may disrupt microbial diversity, potentially increasing CRC susceptibility.3,4 CRC risk is influenced by both genetic predisposition and environmental and lifestyle factors. Individuals with Lynch syndrome or familial adenomatous polyposis (FAP) have a much higher lifetime risk of CRC.
Additionally, genome-wide association studies have identified numerous genetic variants that frequently interact with dietary and microbial factors to increase CRC susceptibility.3
Screening and early detection
CRC is increasingly affecting younger individuals, yet they are often diagnosed at later stages, resulting in poorer outcomes. According to the American Cancer Society, Colorectal Cancer incidence in individuals under 55 has been rising by 1%-2% annually since the mid-1990s, with mortality rates growing at a similar pace.
Patients’ and healthcare providers’ lack of awareness, lower screening rates, misdiagnosed symptoms, and this delay in diagnosis are the primary causes.5,6 Several factors contribute to the late-stage diagnosis of CRC in younger individuals. First, adults have traditionally been the focus of CRC screening guidelines, with routine screenings only being recommended after the age of 45.
Consequently, younger individuals experiencing symptoms such as rectal bleeding or abdominal pain may not seek immediate medical attention, and healthcare providers may not prioritize CRC screening for them. Misdiagnoses, often attributing symptoms to less severe conditions like hemorrhoids or irritable bowel syndrome, further delay detection.5,6
Early screening significantly improves survival rates, with stage I CRC having a 91% five-year survival rate compared to only 14% for stage IV cases. Early detection is enhanced by recent advancements in screening tools like colonoscopies, fecal immunochemical tests (FIT), multi-target stool DNA tests, and FIT.
Artificial intelligence (AI)-assisted diagnostics and liquid biopsies are promising new technologies for improving accessibility and accuracy.5,6 Despite the benefits, screening adherence remains low due to financial constraints, fear, and lack of awareness. Compliance can be improved by expanding screening programs, increasing physician recommendations, and promoting non-invasive tests. Policy changes that remove barriers to cost-sharing for preventive screenings also have the potential to have a significant impact.5,6
Future directions
CRC, which was once thought to be a disease of older people, now increasingly affects people under 50. This trend may be influenced by dietary habits, changes in the microbiome, and genetic predispositions, according to studies. Early detection is being revolutionized by advances in molecular diagnostics like AI-assisted imaging and liquid biopsy. For instance, blood-based tests analyzing circulating tumor DNA (ctDNA) are showing promise as non-invasive diagnostic tools. Additionally, AI is improving the accuracy of colonoscopy screenings, reducing false negatives, and enhancing early intervention efforts.7
A multi-pronged approach to prevention is critical in addressing CRC and other chronic diseases. Lifestyle modifications remain the cornerstone of prevention. Research emphasizes the impact of diet, physical activity, and environmental exposures on CRC risk.
A high intake of processed meats, a lack of fiber, and sedentary lifestyles all play a significant role in the rising number of cancer cases. Conversely, a diet rich in whole grains, lean proteins, and vegetables, coupled with regular exercise, reduces risk.7
Environmental factors also play a significant role. Increased exposure to microplastics, endocrine disruptors, and processed foods affects gut microbiota composition, leading to chronic inflammation. Public awareness campaigns promoting gut health and microbiome diversity through probiotic and prebiotic-rich diets can mitigate risk.7
Policies are being adapted by governments and healthcare organizations around the world to address these growing health issues. In a number of nations, the recommended screening age has been lowered from 50 to 45 due to the rising prevalence of CRC in younger adults.
Participation rates can rise when non-invasive universal screening programs like FIT are implemented. Additionally, disparities in healthcare access are the primary focus of policy reforms. Telemedicine and digital health platforms are expanding preventive care outreach, particularly in underserved populations. Governments are also emphasizing regulatory measures on food labeling, restricting carcinogenic additives, and promoting healthier food environments.1,7
The future of disease prevention lies in integrating scientific research with practical public health strategies and evidence-based policies. A combination of technological advancements, lifestyle modifications, and comprehensive policy changes can significantly curb CRC incidence and improve overall health outcomes.
Strengthening early detection methods, fostering preventive healthcare, and ensuring equitable access to medical resources are essential in shaping a healthier future.



One thought on “Why Colorectal Cancer Is Increasing More Among Young Adults in 2025”